Source: One Healthy Guy’s Mission to Prevent a Diabetes Diagnosis
When my lean, cardio-loving dad developed diabetes, I was shocked to find out the disease could come for me, too. So I set out to see if science could help me change my fate.
IT WAS ABOUT eight years ago when my dad, John Zaleski, first noticed something was off. I’ve always thought of him as someone with an infinite reserve of energy, the sort of stamina that allowed him to work his white-collar job and fix something in the house once he clocked out. This feeling he developed, as he recounted to me this past summer, was different: He felt shaky and fatigued for no obvious reasons. Weariness seemed to attack him out of nowhere. It was a true puzzle—one he started trying to solve when he bought a glucometer, a small device that measures glucose levels. It’s the kind of thing he does, searching for answers to things, even in unlikely places.
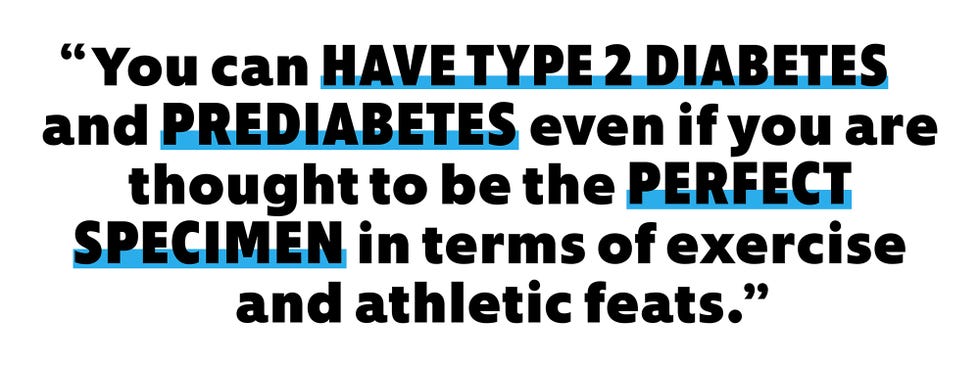
The morning after he picked up the device, he checked his glucose and saw the reading at 218. For perspective, a fasting glucose level of 126 milligrams per deciliter (mg/dl) of blood is considered the threshold for diabetes. The number shocked him. Dad is a lean guy, a trim 150 pounds at five-foot-seven. He regularly exercises (pushups, situps, miles and miles clocked on his Concept2 rowing machine) and works as a volunteer critical-care paramedic with the local fire company and health system in addition to his corporate gig at a large health-care company…where he uses a standing desk. After registering his own fasting glucose, he quickly scheduled an appointment with his primary-care doctor, who ordered blood tests that confirmed the diagnosis: type 2 diabetes.
“I was stunned,” says Dad, who recently turned 60. “I then realized that what I was feeling made sense, but I had no idea that it was diabetes.”
Hearing the backstory for the first time this past summer stunned me as well.
The simple fact that Dad has diabetes places me in a high-risk category, since first-degree relatives are three times as likely to develop it as people without a family history of the disease. It turns out that genetics plays a strong role in its development. “Type 2 diabetes is very inherited,” says Mayer Davidson, M.D., a professor of medicine at Charles R. Drew University and David Geffen School of Medicine at UCLA. Studies of identical twins, for example, have shown that if one twin has type 2 diabetes, the other has a high chance of developing it as well.
In some instances, a family history of obesity can explain someone’s predisposition to type 2 diabetes, since the two conditions are linked: Roughly one quarter of people who have obesity have type 2, and obesity increases your risk of developing the disease threefold. There are also a handful of genes that, if mutated, can increase one’s chances of developing diabetes. But pinpointing one factor—inherited or environmental—as the root cause is a mystery that medicine is still trying to figure out. “There are probably different reasons that different people get it,” Dr. Davidson says. “But we don’t understand any exact causes that we can come up with.”
That’s why type 2 diabetes is usually described as a disease that’s dependent on both genetic and environmental factors, such as what you eat and how you exercise. Just because you have a family history of diabetes doesn’t necessarily mean you’ll develop it, but I didn’t want to find out the hard way.
In a way, I’m somewhat lucky when it comes to my own diabetes prevention, since I’m able to point to something concrete. As I learned three years ago, I have type 1 myotonic dystrophy, an adult-onset form of muscular dystrophy that affects around 40,000 Americans. It’s a genetic disease whose effects may be so mild that someone won’t even know they have it—which was exactly the case with Dad. He didn’t get tested for it until I knew I had it. One of myotonic dystrophy’s hallmarks, regardless of the severity of other symptoms, is insulin resistance, which is one of the ways diabetes starts to develop. And it’s likely how it happened for Dad.
Glucose and insulin play complementary roles in the body. Glucose is our primary source of fuel, the necessary ingredient to help us finish that mile-long run, pump out sets at the gym, or run errands on a Saturday. Insulin, a hormone secreted by the pancreas, breaks down what we eat and releases glucose into the bloodstream. It also helps our cells take in that glucose. But when there’s too much glucose in your bloodstream, the pancreas goes into overdrive to produce more insulin to get those levels down. Eventually, it just can’t keep up, and over time you can develop type 2 diabetes, which can make you feel the way my dad did. Heart disease, nerve damage, impaired vision, and more can follow. (Type 2 shouldn’t be confused with type 1, an autoimmune disorder wherein the pancreas produces little to no insulin at all.)
Admittedly I’d never given diabetes much thought. Like Dad, I’m a trim 150-pound man, albeit 25 years his junior. Preventing the disease was never really a concern of mine until I was sitting in an office at the Johns Hopkins Hospital three years ago, listening to a genetic counselor telling me that I may end up with it. I’m not alone in being at risk of developing diabetes. Close to 98 million Americans—yes, more than one in three adults—have prediabetes, which means their fasting blood sugar is between 100 and 125 mg/dl, and they’re likely to make their way to having type 2 diabetes if they don’t get their blood sugar in check now. As with diabetes itself, prediabetes may be due to genetics or lifestyle factors (and it’s often both). On top of that, about 36 million Americans currently have type 2 diabetes, according to the CDC.
Learning that my ectomorphic body type isn’t guaranteed to protect me from diabetes threw me for a loop. It may just be the case that, one day, my cells won’t respond normally to insulin, increasing my blood-sugar levels to the point where I, too, get type 2 diabetes. How do you outrun your heritage knowing all that? For the past three years, I’ve been trying to figure that out. And I started with the best been-there-done-that expert I could think of: Dad.
THE KEY THING is to maintain your bodyweight in all cases,” Dad’s advice began. “Don’t have a lot of crap in the house.” I know he likes snacks. After all, I’m his son, and when your dad goes hunting for the chocolate ice cream or the cheese puffs, you generally pay attention. (The nights I brought home cheesesteaks and cheese fries probably didn’t help.) But in recent years, he’s radically changed the foods on his plate. The bulk of what he eats now consists of lean protein like chicken and omega-3-rich salmon. He throws back handfuls of blueberries. He cooks with extra-virgin olive oil. Then there’s the asparagus, the Brussels sprouts, and the broccoli.
These days, his fasting glucose numbers generally hover between 108 and 135, aided in large part by his diet—even if he didn’t need to change his weight.
Still, about three quarters of people with obesity do not have type 2 diabetes. And as I discovered on the flip side, not everyone with diabetes has extra weight.
Sandra Arévalo, a registered dietitian and spokesperson for the Academy of Nutrition and Dietetics, says following a prevention diet is a cornerstone of keeping diabetes at bay. In practical terms, that looks a lot like what Dad was telling me. Fill your plate with fresh fruits and vegetables. Pick whole grains and brown rice. When it comes to meat, try to focus on lean meat with little marbling. And then there’s what you don’t want to fill up on. “The number-one recommendation is to limit sugar,” she says. That’s not just the added sugar in everything from ketchup to bread to chocolate-chip cookies. Sugar also refers to refined carbohydrates, like those in white pasta and burger buns and cheese curls, because these carbs turn into blood-glucose-spiking sugars. (Yes, complex carbs like brown rice and bananas eventually turn into sugars as well, just at a healthier, slower rate.)
Refined carbohydrates and added sugar can cause spikes in glucose levels. In the long term, repeated rapid spikes can increase the risk of developing insulin resistance and type 2 diabetes. (After all, you’re asking your pancreas to very quickly pump out insulin to deal with a massive amount of blood sugar—not all of which is going to be taken up by your cells.)
Even for people with a family history of diabetes, these dietary moves can be game-changing. “Genetic predisposition to obesity and type 2 diabetes—these diseases can be prevented by diet and exercise,” says Caroline Apovian, M.D., codirector of the Center for Weight Management and Wellness at Brigham and Women’s Hospital in Boston.
Others who work in diabetes prevention and treatment get more hardcore when it comes to diet. Sami Inkinen is one of them. He’s the founder of Virta Health, a company he created in 2014 with a mission to reverse diabetes in 100 million people. His dive into peer-reviewed research on how to manage blood sugar led him to the work of scientists who were compiling new evidence on the original, pre-insulin treatment for diabetes: a low-carb diet. (Key scientists in this arena—Stephen Phinney, M.D., Ph.D., and Jeff Volek, Ph.D., R.D.—became cofounders of Virta.)
But the low-carb-beats-diabetes approach is a hot button in the diabetes community, with research going back and forth on how effective it is, coupled with affordability issues. A more common approach is following the nutritional guidelines the American Diabetes Association recommends for type 2 prevention and management. When I reached out to ask about the best diet for both preventing my type 2 and, maybe one day, managing it, I was given a blueprint for my dinner plate by Toby Smithson, R.D.N., the association’s senior manager of nutrition and wellness.
Grab a nine-inch plate, she says, and cut it in half, filling one half up with stuff like broccoli, green beans, and cauliflower. Then cut the other half of the plate in half. Fill the top with lean proteins like chicken and fish and the bottom with complex carbohydrates like sweet potatoes and quinoa, anything that takes a while to break down into sugars in the blood.
Thanks to Dad, I already tend to do this pretty well: smoked salmon and baked chicken, broccoli, brown rice, green beans, arugula. I like eating red grapes and Cosmic Crisp apples more than the blueberries Dad favors, but sometimes I eat those, too. And I should probably swap fatty rib eye steaks for strip steaks when I do eat red meat. More recently, though, I’ve begun considering cutting more carbs from my diet. The last time I had my fasting glucose checked, in March following my annual checkup, my number was 95, squarely in the healthy range. If it goes higher, I’ll probably be much more careful about what I’m putting on my dinner plate.
With that in mind—and with my weight-management strategy, evidently, well in hand—I looked at what could shift my diabetes-prevention strategies into overdrive.
NORMALLY, THE MUSCLES in our body are a massive sink for excess glucose. The ADA recommends that people do some strength training two or three times a week. More muscle mass means your body can better deal with any glucose floating around.
Having muscular dystrophy makes this recommendation a little more complicated at both the biological and practical levels. In my body, most of the insulin receptors contained in muscle tissue are spliced abnormally, making them insulin insensitive. My pancreas is already working harder to pump out more insulin than normal in order to get my cells to gobble up excess glucose.
For specific guidance, I spoke with John W. Day, M.D., Ph.D., the director of Stanford’s Division of Neuromuscular Medicine and a medical advisor with the Muscular Dystrophy Association. The main thing is focusing on what might increase my risk of getting type 2 and then minimizing it. “And so what are the things that are going to precipitate that risk?” he says. “More sedentary activity as opposed to more active activity.” Put another way: Don’t stay seated the whole day.
My own doctors tell me I shouldn’t lift weights anymore, since my body is slowly losing the stem cells that help regenerate muscle tissue. Bodyweight exercises for me, though, are fair game, as is any sort of aerobic exercise my legs can tolerate. Dr. Davidson says aerobic exercise means getting my pulse up to 70 percent of my maximal heart rate and doing it three times a week. Translated, that means getting my heart rate up to a point where I can carry on a conversation but talking might take a little more effort than usual.